Overview
Blood banks of all types use anti-coagulants to combat the coagulation of blood and provide the cells inside with nourishment. While there are a number of different anti-coagulants available, most cord blood banks use one of two: CPD or heparin. Between the two, CPD is the only one recommended by the FDA and preferred by experts in the field. It has been found that cord blood held in collection bags that have liquid CPD appear to contain significantly more stem cells and white blood cells than cord blood held in collection bags that use dry heparin. It is important for parents who are planning to bank their baby's cord blood to ask the cord blood bank what type of anti-coagulant it uses in its cord blood collection bag.
Anti-Coagulants Explained
Blood isn't designed to be held outside the body, where it immediately begins to coagulate and dry. To prevent this from occurring, cord blood banks, like other types of blood banks, use substances in their cord blood collection bags to prevent the components of blood from forming a gel-like solid.
Coagulation Cascade
Coagulation is a series of events, each one spurring the next and amplifying the total response; it is a domino effect. It begins with the activation of molecules in the blood and ends with the attraction of blood platelets to the site of the wound and the formation of a spider-like web of fibrin that catches red blood cells and forms a scab. The whole series of events play out like a Rube Goldberg machine and has been dubbed the cascading effect.
The activation of the clotting process comes from factors in the damaged tissue but can also begin when the blood comes into contact with substances outside the body. Once these molecules are activated, the contents of any collection of blood could be lost.
There are other reasons blood cannot sit indefinitely inside of a collection bag. Cord blood continues to "live" after it has been extracted from the umbilical cord, but it is missing the bodily functions that supply it with energy and dispose of waste. Specifically, the red and white cells are still metabolizing glucose and creating lactic acid. Lower temperatures keep the rate of glycolysis at a lower limit, (This is why the cord blood's stem cells and white cells are cryo-preserved at temperatures of −310 degrees Fahrenheit; it effectively stops any chemical reactions that could damage the cells.) but up until cord blood can be cryo-preserved, it must be kept safe during transportation.
Anti-Coagulants

Collection bags like this come pre-filled with 35 mL of CPD anti-coagulant.
Anti-coagulants are used in the cord blood bag to keep the coagulation cascade from occurring and to supply the cells with nourishment while helping to minimize the effects of waste. It provides a larger window of opportunity to keep the blood stabilized. While there are a number of different anti-coagulants used in blood products, most cord blood banks either use a citrate-based anti-coagulant, as recommended by the FDA, or heparin.
Citrate-Based
Citrate is a common component of anti-coagulants. It is a calcium-bonding agent that prevents coagulation by interfering with the calcium-dependent steps.
Sodium citrate has been used since the 1890s and is widely considered to be effective and non-toxic. Citrate–dextrose solutions were used in the first blood banks set up during World War I. In 1943, acid–citrate–dextrose (ACD) was developed, and in 1957, ACD's less-acidic replacement, citrate–phosphate–dextrose (CPD), was introduced. ACD and CPD give cord blood a shelf life of 21 days. Developed in the 1970s, CPDA-1 adds adenine, which aids cell metabolism, and gives blood a shelf life of 35 days.
Heparin

Heparin is mainly derived from pig intestines.
Another type of anti-coagulant was discovered in dog livers by Jay McLean in 1916 and named heparphosphatid. It was later re-named heparin. Heparin has been continually purified through the years and is mostly procured through pigs. It works by binding to anti-thrombin and blocking the clotting cascade, but it comes with its drawbacks. Heparin can begin breaking down within 12 hours and start to lose its anti-coagulant properties, and as it is an animal product, it may be contaminated with bacteria and viruses. It can also affect the matching process that allows doctors to know if a recipient and donor are compatible for a blood transplantation.
Cord Blood Banking
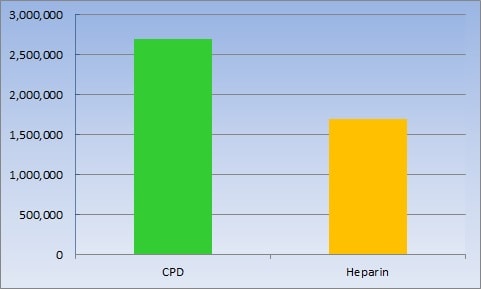
CPD versus heparin in CD34+ (stem) cell count
Because of heparin's drawbacks, CPD has been nearly unanimously chosen as the best anti-coagulant for cord blood banking. The FDA, which had to administer a large recall on some heparin products in 2008 because of contamination, recommends citrate-based anti-coagulants such as CPD. In addition, liquid CPD is the preferred anti-coagulant of Dr. Joanne Kurtzberg, a well-respected researcher at Duke University Medical Center, and Pablo Rubenstein, the founder and current director of the National Cord Blood Program, the first public cord blood bank. It is the type of anti-coagulant used by us here at Cryo-Cell as well as other prominent cord blood banks.
CPD does not start to break down and lose its anti-coagulating effects as heparin does; it is not an animal product and is not likely to have been exposed to bacteria and viruses as heparin has and it does not bear upon the HLA markers used for matching as heparin does. In a study, cord blood collected in a bag with liquid CPD had 30 percent more total nucleated cells (i.e., white blood cells) and 58 percent more CD34+ cells (i.e., stem cells) than similar collections with heparin.
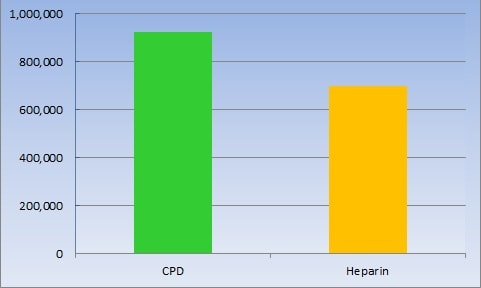
CPD versus heparin in total nucleated (white) cell count
Unfortunately, as citrate-based anti-coagulants are not required but just recommended by the FDA, there are cord blood banks that use lyophilized, or dry, heparin in their cord blood collection bags. There has even been "research" sponsored by some supporters of heparin to devalue the benefits of CPD. This research says the dilution of CPD to blood could have an adverse impact on cell viability and blood chemistry in low-volume collections. As there is approximately 35 milliliters of CPD in the cord blood collection bag, it says that a ratio of 1:1 could negatively affect the collection. The fact is that such a small volume of cord blood would not likely carry the number of stem cells for transplantation and that there is no evidence that the volume of CPD anti-coagulant affects the final cell product to any significant degree.
As the drawbacks to heparin and benefits of CPD are clear, it is important for people who are going to bank their cord blood to make sure their baby's stem cells are collected in cord blood bag with a citrate-based anti-coagulant. The table below shows which leading cord blood banks currently use a citrate-based anti-coagulant:
| |
Cryo-Cell |
ViaCord |
Cord Blood Registry (CBR) |
| Collection bags with citrate-based anti-coagulants |
 |
 |
 |