September is National Sickle Cell Awareness Month, and if there is one action that can have a lasting impact on the disease, it is cord blood banking.
A short primer on sickle cell disease
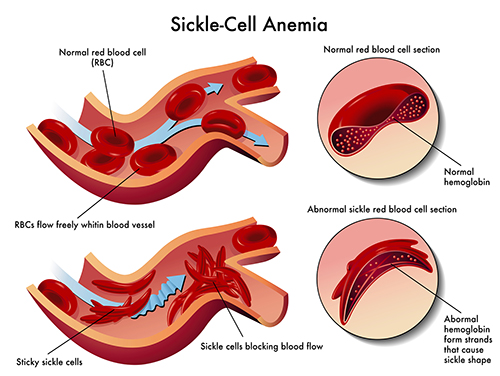
Inside sickle cell anemia
Sickle cell disease (SCD) is a genetic blood disorder that’s inherited—it’s passed from parents to children. Babies are born with sickle cell disease when they inherit two abnormal genes, one from each parent. A baby who inherits one abnormal gene from one parent is a carrier; they will have the sickle cell trait. If that baby grows up to have a child with another carrier, then their baby might have sickle cell disease.
Complications of sickle cell disease
The sickle cell genes cause episodes where the body’s red blood cells become rigid, inflexible and mis-shaped, changing from a disk shape to a curved shape that looks like a crescent moon or an old farm tool known as a sickle. These “sickle” cells tend to stick together and block the flow of blood and oxygen to the body, causing pain in the extremities and back, infections in the skin and other areas, organ failure and other tissue damage, loss of eyesight, severe blood clots and strokes. These complications tend to progress at adolescence and worsen during early adulthood and often lead to early mortality.
In addition, the sickle-shaped blood cells don’t last as long as they do in healthy people (10–20 days as opposed to 120 days). The bone marrow can’t replace these blood cells fast enough, which causes anemia.
Sickle cell can also lead to infections in the spleen. As the spleen filters the blood of infections, it can filter out the sickle-cell shaped red blood cells. This can cause the spleen to become overworked and eventually start to fail.
What is the differences among sickle cell trait, sickle cell anemia and sickle cell disease?
Sickle cell trait is when a person has inherited the gene from one parent and could possibly pass the disease along to any offspring. Sickle cell anemia is when the person has received the sickle cell gene from both parents. Sickle cell disease is a more general term to describe sickle cell anemia and other conditions where a sickle cell gene and another gene that causes abnormalities in the red blood cells is inherited. For example, sickle cell–beta thalassemia is the combination of a sickle cell gene and beta thalassemia, a blood disorder that reduces the production of hemoglobin, the iron-containing, oxygen-carrying part of the red blood cell that also helps it retain its disk shape.

SCD is more common in African Americans and Hispanic Americans
Who is affected by SCD?
Sickle cell disease (SCD) is particularly common among those whose ancestors came from sub-Saharan Africa; Spanish-speaking regions in the Western Hemisphere (South America, the Caribbean, and Central America); Saudi Arabia; India; and Mediterranean countries such as Turkey, Greece, and Italy.
How common is SCD?
SCD affects approximately 100,000 Americans. It is, however, more common among African American and Hispanic Americans:
- SCD occurs among about one out of every 365 black or African–American births.
- SCD occurs among about one out of every 16,300 Hispanic–American births.
- About one in 13 black or African–American babies is born with sickle cell trait (SCT).
Treating sickle cell disease
Antibiotics and pain-relievers can be used to help treat the symptoms of sickle cell anemia and other sickle cell diseases and prevent any infections, but the only potential cure is a transfusion of stem cells like those found in cord blood. This procedure first requires the patient to receive a drug that will wipe out his or her blood-forming bone marrow stem cells. The transfusion then replaces the old bone marrow with new, healthy stem cells, which will produce normal red blood cells.
Finding a matching unrelated bone marrow donor can be difficult, and any time stem cells come from an unrelated source, they have a high risk of causing graft-versus-host disease. Luckily, siblings are prime candidates because once parents have a child with a recessive sickle cell trait or disease, every subsequent child has a 75 percent chance of not having the trait or disease. This makes every subsequent birth a good opportunity to store the baby's cord blood to treat the other child's sickle cell disease.
A recently completed large-scale analysis shows that cord blood and other related transplants are successful in most children with sibling donors. The study looked at the results of 1,000 patients, with an average age of nine years old. The three-year overall survival rate was 99 percent for patients who received donor cord blood, 94 percent for those who received donor bone marrow and 80 percent for those who received transplanted peripheral blood. (Read more about cord blood's advantages over bone marrow here.)
This study strengthens several earlier studies, attesting to the excellent outcomes of cord blood transplants to treat sickle cell disease. An earlier National Institute of Health (NIH) study showed that the possibility of treatment for adults suffering from sickle cell anemia has greatly improved. Matched-sibling donors showed a high success rate for a cord blood–like transplant therapy.
The National Institute of Health's Dr. Matthew Hsieh and his team disproved the hypothesis that adults are too likely to reject the stem cell transplant because of toxicity. The creative and effective therapy used in the study solved this obstacle with impressive success.
Conclusion
The best treatment for a child with sickle cell disease is a sibling's cord blood because of the high probability that the sibling will not carry the sickle cell trait or disease. In addition, sibling cord blood has been shown to have the highest survival rate compared with other stem cell sources like bone marrow. This makes cord blood banking especially important for African Americans and Hispanic Americans, who have a higher chance of inheriting sickle cell disease.
First published in July 2014. Revised and re-published in September 2016 and in August 2017.